Pilonidal cysts
What is a pilonidal cyst and how does it develop?
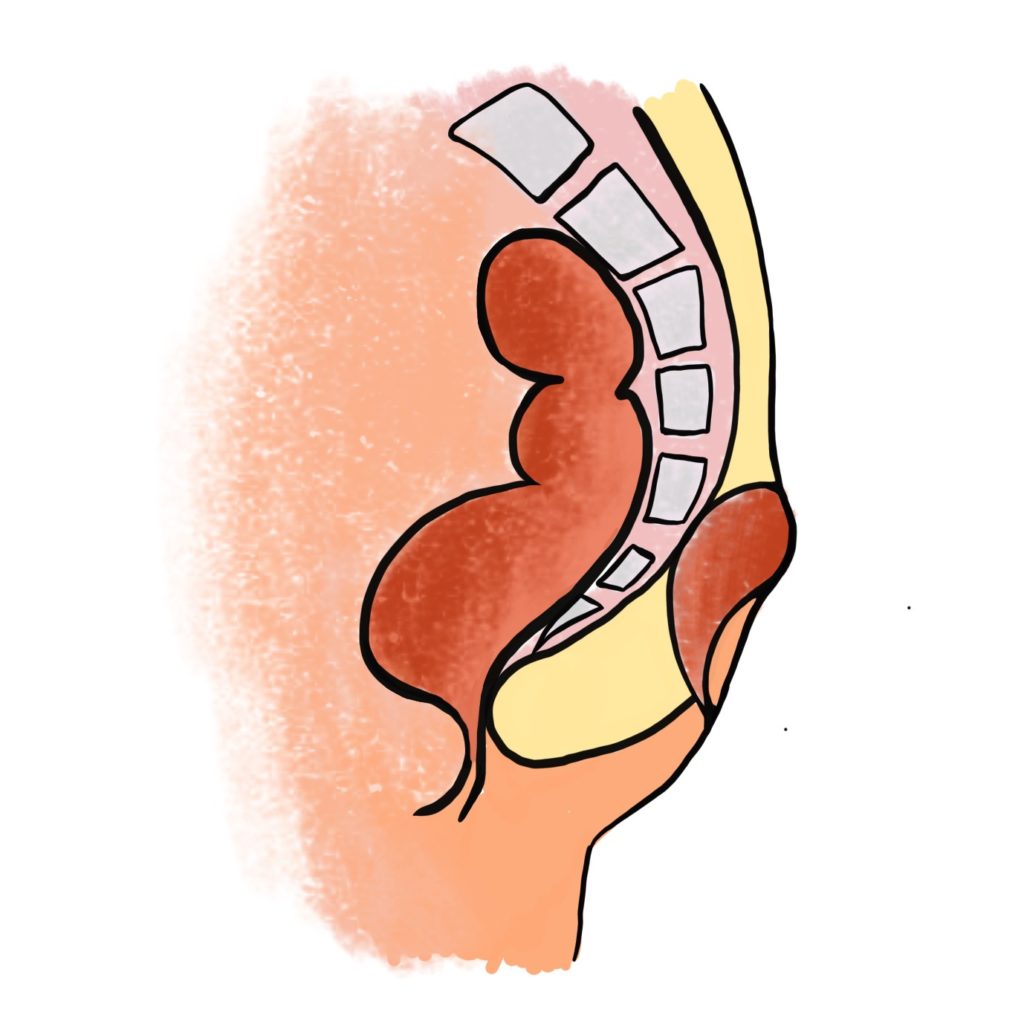
A pilonidal cyst is a chronic abscess of the subcutaneous tissue, located at the bottom of the intergluteal cleft. The characteristic feature of the cyst is the presence of hair in the cavity of the fistula, however this is not always the case. Pilonidal cysts (fistulas) often appear in adolescence. They are far more common in males.
There are numerous theories on the development of the pilonidal fistula. The most probable one is the damage of skin at the bottom of a tight and deep intergluteal cleft caused by sweat and mechanical abrasion. Skin damage leads to secondary infection of the superficial wounds, and then the penetration of bacteria to the subcutaneous tissue followed by the formation of an abscess cavity connect to the skin surface by one or more skin fistulas.
Despite the common ingrown hair theory, studies have shown that the hair collected from the pilonidal fistula mostly come from the head. Often, this is the hair cut by a hairdresser – short, stiff and with sharp endings, which penetrates into the cyst through the damaged skin and skin fistulas.
Pilonidal cyst duct
1 of 1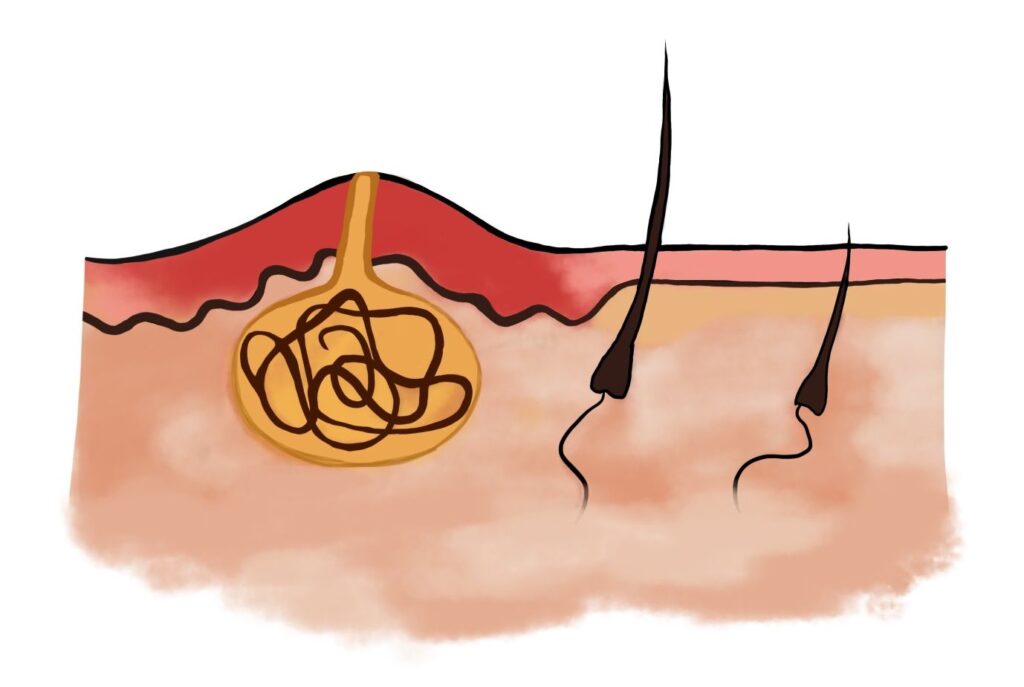
Ingrown hair
1 of 1
Clinical picture of pilonidal disease
Depending on the stage, the condition may be asymptomatic or may present as a recurrent, complex cyst. The course of the condition, when untreated, involves periodic acute infections causing pain, edema, and reddening of the intergluteal area, sometimes accompanied by a high fever. Due to the tightness of the intergluteal cleft, the abscesses often penetrate upward, and usually move to the buttock, where they open outside of the intergluteal cleft.
Following abscess evacuation, remission may last for several months or years. Inflammatory infiltrate and the pain subside, a serous or purulent discharge, often tinted with blood, may persist.
The hair inside the pilonidal cyst irritates the subcutaneous tissue and prevents the abscess cavity from healing fully. The continuously irritated tissue is surrounded with a scar capsule that can be felt through the skin and is filled with thick, mucous-like fluid and granulation tissue.
Due to the long and difficult healing process and the risk of recurrence, patients often suffer for many years, experiencing discomfort and a feeling of embarrassment.
Diagnosis and qualification for pilonidal cyst treatment
During the qualification visit, Dr. Norbert Zapotoczny assesses the lesion and establishes the final diagnosis based on the patient’s symptoms and the ultrasound. Then he discusses possible treatment methods with the patient. Each of the methods has its advantages and disadvantages, which is why discussing all the pros and cons with the patients is so important, since everyone may have different expectations and priorities regarding the treatment effects.

There are numerous methods of pilonidal cyst treatment that differ both in terms of wound healing duration, quality of life after surgery, and the risk of recurrence.
When planning pilonidal cyst treatment, we focus on three main objectives:
1. Wound healing
Wound healing should be as fast as possible and wound care should be easy and not require the help of nurses but merely some assistance of family members.
2. The quality of life
The quality of life after surgery should be high enough for the patient to be able to function relatively normally, sit down, take a shower, sleep in supine position, drive, walk, and perform work that does not require major physical effort.
3. The risk of recurrence
The risk of recurrence should be as low as possible.
The esthetic aspect
The esthetic aspect is also important – the postsurgical wound area and the shape of the buttocks should remain as close to natural as possible, the scar should be as little visible as can be; vast and wide scars should be avoided, especially those running across the intergluteal cleft.
Each of the treatment methods has its advantages and disadvantages, which is why discussing all the pros and cons with the patients is so important, since everyone may have different expectations and priorities regarding the treatment effects.
The consequences of untreated pilonidal disease
Lack of adequate treatment may result in painful symptoms. In the acute phase, symptoms of acute systemic inflammation develop, with strong pain in the affected area, fever, chills, and reddening of the skin in the sacral-coccygeal region.
In the chronic phase, a pilonidal disease is usually asymptomatic for many years; periodically a purulent or bloody-purulent discharge with an unpleasant smell is produced. Considering the above symptoms and in order to obtain a detailed diagnosis, it is recommended to visit a surgeon who will assess the lesion with ultrasound imaging and provide final diagnosis.